Turner Syndrome: More Than a Missing “X”
- What Is Turner Syndrome (TS)?
- What Causes Turner Syndrome?
- How Is Turner Syndrome Diagnosed?
- Common Turner Syndrome Symptoms
- What Medical Problems Are Common in TS?
- Growth and Development
- Do Females With TS Have Other Medical Issues?
- The Cardiovascular System (Heart and Blood Vessels)
- Bones and Joints
- Metabolism
- Kidneys and Urinary Tract
- The Immune System
- Thyroid
- Celiac Disease
- Juvenile Rheumatoid Arthritis
- Chronic Inflammatory Bowel Disease
- Eyes and Vision
- Ears and Hearing
- Dental Problems
- Skin Problems
- The Lymphatic System
- Cancer
- Treatments for Turner Syndrome
- Fertility and Family-Planning Issues for Women With TS
- The Bottom Line
Key Takeaways
- Turner syndrome (TS) is a condition that affects girls and women.
- TS is characterized by short height, lack of sexual development, webbing on the neck, and arms that angle outward at the elbows.
- TS can cause delayed puberty and increase the risk for various types of medical problems.
- Thanks to medical advancements, girls and women with TS can experience normal puberty and enjoy healthy, productive lives.
What Is Turner Syndrome?
When a set of features or symptoms occur together and are believed to have the same cause, it is referred to as a “syndrome.”
Turner syndrome was first described in 1930 by a geneticist named Otto Ullrich when he noticed certain physical characteristics in an 8-year-old girl. Eight years later, Dr. Henry Turner from Oklahoma published a report describing seven female patients who had the same characteristics:
- Short stature (height)
- Lack of sexual development
- Extra folds of skin extending from the tops of the shoulders to the sides of the neck (referred to as webbing)
- Arms that angle outward at the elbows (known as cubitus valgus)
Dr. Turner named this set of symptoms Turner syndrome (TS). It wasn’t until 1959 that Dr. C.E. Ford discovered that TS is a genetic condition involving the sex chromosomes.
Turner Syndrome affects one in every 2,500 females born. It is a random genetic error that occurs when the egg and sperm come together to form a baby. Turner Syndrome is not related to the age, ethnicity, diet, or actions of the parents. Nothing can be done to prevent Turner Syndrome.
Very few pregnancies in which the fetus has TS result in live births. The majority, 99%, end in early pregnancy loss (miscarriage).
What Are Sex Chromosomes?
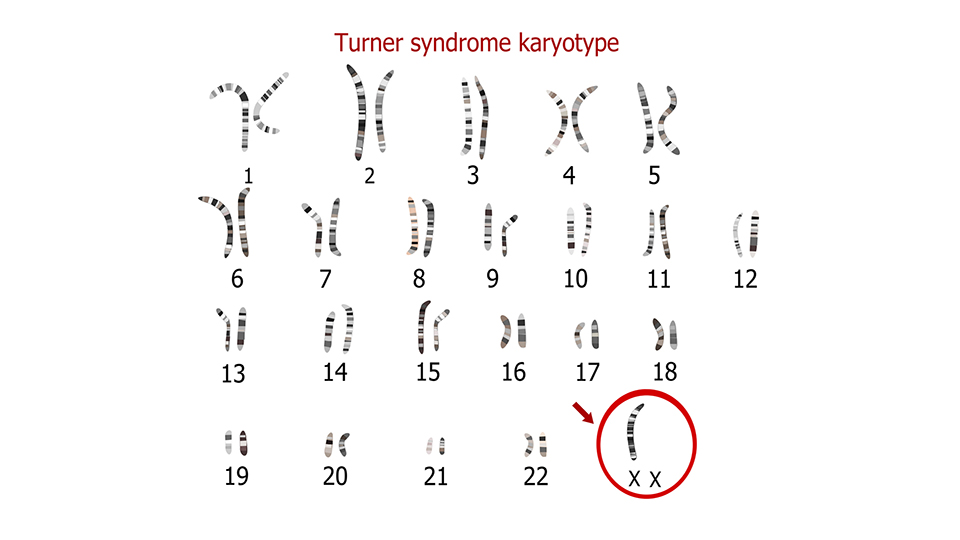
The human body is made up of millions of cells. Inside each cell, there are 23 pairs of chromosomes—DNA molecules that are responsible for transferring genetic information from one generation to the next.
Humans have two types of chromosomes:
- Sex chromosomes: Each person has one pair.
- Autosomes (chromosomes that are not sex chromosomes): Each person has 22 pairs.
There are two sex chromosomes: the X chromosome and the Y chromosome. These chromosomes determine the biological sex of a person. A male child inherits a Y chromosome from his father and an X chromosome from his mother. A female child inherits two X chromosomes, one from each parent.
The X and Y sex chromosomes contain many genes that are responsible for the development of the sex organs and physical characteristics associated with male and female biological sexes. Two X chromosomes are necessary for the normal growth and development of biological females.
What Causes Turner Syndrome?
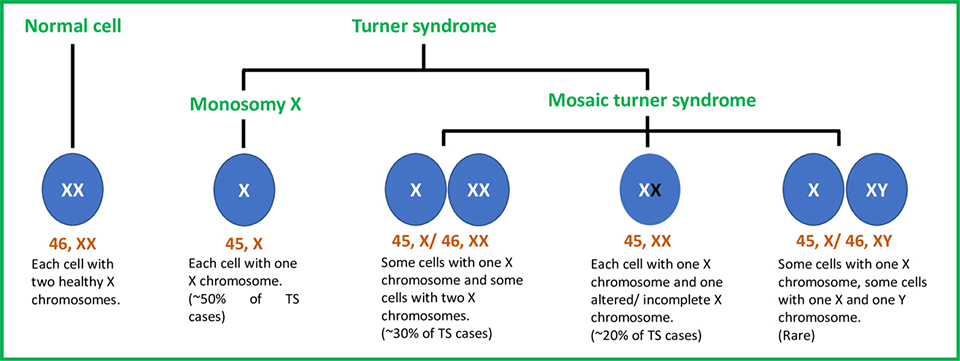
Turner syndrome is a chromosomal condition related to the X chromosome. It occurs when a girl has one normal X chromosome, but the second X chromosome is either missing, incomplete, or altered.
Mosaic Turner Syndrome
About 50% of girls with TS are missing one of the usual two X chromosomes in every cell. This is known as 45, XO, or monosomy X.
About 30% of girls with TS have some cells that are complete with two X chromosomes (46, XX) and some cells that are missing an X chromosome (45, X). This is called mosaicism or mosaic Turner syndrome.
Another less common mosaicism is 45, X/46, XY. People with this type of TS have some cells containing only one X chromosome, as well as cells that contain both an X chromosome and part of the Y chromosome. This type of mosaicism can increase your risk of developing reproductive organ tumors called gonadoblastomas. Girls who have a 45, X/46, XX mosaicism tend to have fewer features of TS, making diagnoses more difficult.
About 20% of girls with TS have two X chromosomes in each cell, but one of them is altered or incomplete.
How Is Turner Syndrome Diagnosed?
A combination of physical exams and laboratory genetic tests is used to diagnose TS.
Prenatal Diagnosis (Before Birth)
TS can be diagnosed during pregnancy. If a prenatal ultrasound shows that the baby has physical features common to TS, a karyotype may be performed to confirm the diagnosis.
Karyotyping is testing used to determine your genetic makeup. In order to determine the genetic makeup of a fetus, doctors need to test the mother’s amniotic fluid (amniocentesis) or take a small portion of the pregnancy tissue (chorionic villus sampling or CVS). These tests are more accurate than ultrasounds. However, they are also more invasive, so they carry a higher risk of pregnancy complications.
Diagnosis in Infancy
Newborns may be diagnosed with TS through karyotype testing. This is usually done through the blood.
If a diagnosis of TS was not suspected before birth, your pediatrician might request testing if your baby shows certain features common among girls with TS. Common clues that may indicate a diagnosis of TS are heart problems along with certain physical features, such as swollen hands and feet, excess skin around the neck (webbed neck), widely spaced nipples, and low-set ears.
Diagnosis During Childhood and Adolescence
Some girls do not have obvious physical signs of TS at birth and may not be diagnosed until childhood. Children with TS tend to grow very slowly. Half of girls with TS will be smaller than 95% of their peers by age 2. Clues that develop later include lack of breast development, no menstruation, and no pubertal growth spurt.
Diagnosis During Adulthood
In a small number of women with TS, puberty occurs naturally. Later, however, their ovaries stop functioning, and they become menopausal sooner than expected. This is known as early menopause or premature ovarian failure.
Other women with TS may experience unexplained infertility. Hormone tests may suggest TS, but a karyotype must be done to confirm the diagnosis.
Common Turner Syndrome Symptoms
The symptoms and severity of Turner syndrome can vary from one person to another. Many features of the disorder can be subtle and may be caused by multiple medical conditions. Some girls with TS may not show all its signs or symptoms.
One feature seen in most girls with TS is poorly developed ovaries. Since the ovaries produce the sex hormones necessary for puberty, without treatment, girls with TS fail to develop breasts and pubic hair and do not menstruate. Girls with TS also experience infertility.
Almost all girls with Turner syndrome experience growth failure. If untreated, the final height of females with Turner syndrome is usually under 5 feet.
Common Features of Turner Syndrome
Common signs and symptoms of Turner syndrome include:
- A wide, webbed neck (neck with excess skin).
- A low or indistinct hairline in the back of the head.
- Swelling of the hands and feet (known as lymphedema).
- A broad chest and widely spaced nipples.
- Arms that turn out slightly at the elbow (known as cubitus valgus).
- Congenital (at birth) heart defects or heart murmur (up to 50% of cases).
- Scoliosis (curving of the spine) or other skeletal abnormalities.
- Abnormal kidneys (30–50% of cases).
- Drooping eyelids or a “lazy eye.”
- Small jaw without a prominent chin.
- Crowded teeth.
- Multiple moles.
- Low-set, prominent ears.
- Stocky appearance.
- Wider upper body than lower body.
- ”Short” ring finger (the hand bone that joins the ring finger is short, not the finger itself).
- Soft, narrow fingernails and toenails that point upwards.
What Medical Problems Are Common in TS?
Growth and Development
There are three areas that are often of concern in girls with TS: growth, sexual development, and the development of skills required to do well in school and in relationships.
Growth
Short stature (height) is the most common feature of TS. Girls with TS begin to display poor growth at around 1.5 years. By age 3.5, 75% of girls with TS are shorter than 95% of their peers. Many girls with TS have a delayed bone age, which means that their bones are more like those of younger girls.
Female hormones (estrogens), which are made by the ovaries during puberty, speed up bone growth and maturation. Most girls with TS who are not treated with hormones will not have a pubertal growth spurt and may continue to grow at a slow rate until they are in their twenties. The average adult height of an untreated woman with TS is 4’8” (142 cm), although some women reach 5’ (152 cm).
All girls with TS should have their growth carefully and regularly tracked on the TS growth chart. Current guidelines recommend considering growth hormone treatment once a girl’s height drops below the 5th percentile on the standard growth chart. This means that all girls with TS who are shorter than 95% of their peers should receive hormone therapy—even if they are as young as 2 years of age.
Sexual Development
Another hallmark feature of TS is a lack of sexual development (breast development, feminine body contours, and menstruation).
The ovaries have two major functions:
- Produce the female sex hormones estrogen and progesterone.
- Store eggs and release them on a regular basis once menstruation begins.
The ovaries of girls with TS are often abnormal and do not function. As a result, sexual development will not occur unless the female sex hormones are replaced with medication (hormone treatment). Sexual function is normal in women with TS who are receiving hormone treatment.
In TS, the ovaries do not develop eggs, so spontaneous pregnancy is rare and carries a high risk of genetic problems in the baby. The other female reproductive organs (fallopian tubes, uterus, and vagina (birth canal) are present and function normally, so pregnancy with a donor egg and in vitro fertilization (IVF) is possible in adulthood.
Intelligence and Academics
The intelligence of girls with TS is usually in the normal range. However, girls with TS are more likely than other children to have specific learning disabilities, mostly non-verbal learning disabilities (NVLD). These can involve:
- Difficulty imagining objects in relation to each other (visual-spatial processing; difficulty driving and poor sense of direction).
- Trouble appreciating subtle social cues such as facial expressions (social cognition).
- Problems with nonverbal problem-solving (math).
- Clumsiness (psychomotor problems and poor manual dexterity).
If a learning disability exists, occupational therapy, academic tutoring, and training in problem-solving can help girls with TS cope with visual-spatial and learning challenges.
The results of early research on adults with TS show that they are less likely than other women to live independently, marry, and be sexually active, in spite of similar education and employment backgrounds. This shows the importance of attending to social and emotional development in childhood and adolescence.
Do Females With TS Have Other Medical Issues?
There are a number of health concerns and medical problems that occur more frequently in girls with TS than in other children. The severity of these conditions can vary, with some girls being seriously affected, some mildly affected, and others not affected at all.
The Cardiovascular System (Heart and Blood Vessels)
Congenital heart disease (heart disease present at birth) occurs in up to 50% of individuals with TS. It is the most frequent cause of early mortality in those with the syndrome.
Common heart abnormalities seen in TS include:
- Narrowing of the aorta (the large, main artery leaving the heart). This problem is called coarctation of the aorta and is found 7–18% of the time in TS.
- Abnormalities of the valve that connects the aorta with the heart. This is referred to as a bicuspid aortic valve, in which the aortic valve has only two flaps (leaflets) instead of the normal three. This occurs 15–30% of the time in TS.
All girls with TS should undergo a cardiac evaluation at the time they are diagnosed, regardless of age. Screening may include an echocardiogram (ultrasound) or MRI of the heart. Cardiac screening should take place again in adolescence, and then every 3–5 years as an adult.
Hypertension (high blood pressure), coronary heart disease, and stroke are major factors that can reduce the lifespan of an individual with TS. Hypertension rates are 20–40% in children and 60% in adults.
The heart defects associated with some cases of TS can increase the risk of severe, life-threatening complications, including:
- High blood pressure of the lungs (pulmonary hypertension).
- Aortic root dilatation (enlargement of the large blood vessel that carries oxygenated blood from the heart). This is often associated with weak muscles in the wall of the aorta. The weak muscles can cause the walls to tear, then separate (aortic dissection) or burst (aortic rupture), causing internal bleeding, shock, and possibly death.
Women with TS are at an increased risk for heart-related complications during pregnancy. These include tearing of the aorta and hypertension-related disorders of pregnancy, like preeclampsia.
Bones and Joints
Bone and joint abnormalities are extensive in TS, though they can vary from person to person. Developmental hip dysplasia can cause the development of arthritis of the hips in individuals with TS as they age. 10% of girls with TS will develop scoliosis (curved spine), kyphosis (bending forward of the spine), or lordosis (an excessive curve in the lower, or lumbar, spine). Abnormalities in knee alignment (being “knock-kneed”) and the arches of the feet are also common and can cause pain.
Many women with TS have osteoporosis (weakened bones). This, along with low estrogen levels and abnormal vitamin D metabolism, can increase the risk of bone fractures (breaks). Osteoporosis may improve for those who receive growth hormone during childhood, start estrogens during early adolescence, and take estrogens regularly during adulthood.
Metabolism
Obesity is a common problem in TS, especially during adolescence and adulthood. Diet and exercise are the keys to weight control in TS, just as they are for all of us.
Turner Metabolic Syndrome
Girls and women with TS are also at increased risk for a group of conditions called metabolic syndrome. These include:
- High blood pressure.
- Abnormal blood lipids (cholesterol, triglycerides).
- Non-insulin-dependent diabetes (NIDDM).
- Obesity.
- Increased insulin secretion and insulin resistance.
Kidneys and Urinary Tract
Kidney anomalies, or abnormal changes to the kidneys, affect 30–40% of females with TS. Deaths related to kidney disease are 7 times higher in women with TS than in the general population.
- 11% have horseshoe-shaped kidneys.
- 5–10% have partially or totally duplicated kidneys.
- 2–3% have one absent kidney.
- Less than 1% have multicystic or ectopic
Urinary tract infections (UTIs) are thought to be more frequent in girls with TS due to blockages, or reflux, of urine flow. Prolonged reflux or recurrent infections can lead to kidney scarring, which, in turn, can result in elevated blood pressure.
The Immune System
Individuals with TS have an increased risk of autoimmune diseases. Your body’s immune system protects you from disease and infection. If you have an autoimmune disease, your immune system attacks healthy cells in your body by mistake.
Thyroid
The thyroid is a gland in the neck that belongs to the endocrine system. It helps regulate the body’s metabolism.
Autoimmune thyroid disease, called Hashimoto’s autoimmune thyroiditis, is common during childhood in TS and has been reported as early as age 4. Between 10 and 30% of females with TS will develop hypothyroidism (underactive thyroid) because the thyroid becomes less able to produce thyroid hormones.
Females with TS should have blood work done annually starting at age 4 to check for the development of thyroid problems.
Celiac Disease
Celiac disease is an autoimmune disorder. It causes the immune system to be abnormally sensitive to gluten, a protein found in wheat, rye, and barley. The risk of celiac disease is increased in TS, affecting 4–6% of individuals with the condition (as opposed to 1% in the general population). Periodic screening blood work should begin at age 4 and be repeated every 2–5 years.
Juvenile Rheumatoid Arthritis
Girls with TS may develop juvenile rheumatoid arthritis (JRA). JRA is a form of autoimmune arthritis that first appears before the age of 16. It may involve joint pain or inflammation, as well as eye inflammation, fevers, or rash.
Chronic Inflammatory Bowel Disease
There is a high incidence of chronic inflammatory bowel disease (IBD) in TS. Girls and women with TS are at an increased risk of developing Crohn’s disease or ulcerative colitis. These autoimmune disorders attack the intestines, causing chronic swelling, inflammation, and pain.
Eyes and Vision
Girls and women with TS may develop certain vision problems. Astigmatism (abnormally shaped cornea), near-sightedness, and far-sightedness occur more frequently in those with TS than in others.
Strabismus (abnormal eye alignment or crossed eyes) affects about one-third of those with TS. It usually becomes evident between 6 months and 7 years of age. If not treated promptly with special glasses or surgery, 30–50% of those affected will experience decreased vision in the wandering eye(s). Amblyopia (“lazy eye” with decreased vision), unusual eyelid folds, and ptosis (droopy upper eyelid) are also more common in TS.
Red and green color blindness or color vision abnormalities occur in 8% of females with TS. Congenital glaucoma (increased pressure inside the eye starting at birth) and cataracts in older women also seem to occur more in TS.
Annual eye exams are recommended starting at 2 years old to help detect and correct any vision problems.
Ears and Hearing
While it does not affect hearing, TS is commonly associated with low-set ears and a wide, short ear canal. Middle ear infections (otitis media) occur frequently in TS, especially during infancy and early childhood.
Recurrent middle ear infection (chronic otitis media) may lead to hearing loss. Hearing abnormalities in young children may affect or delay speech development. Early recognition, evaluation, and treatment of hearing impairment are crucial in order to avoid hearing-related speech problems. Fortunately, hearing loss due to chronic ear infection usually resolves as girls get older and ear infections become less frequent.
Sensorineural hearing loss occurs when the ability of the auditory nerves to transmit sounds to the brain is impaired. This is common in adults with TS, affecting 90% of women in their 40s, and may worsen with age. More than 25% of those with TS experience sensorineural hearing loss and will eventually require hearing aids.
A formal hearing test is recommended every three to five years if you have TS.
Dental Problems
Individuals with TS may have a wide range of dental and orthodontic issues, including:
- Baby teeth and permanent teeth appearing earlier than usual.
- Increased risk for root shortening, which can lead to tooth loss, especially during orthodontic treatment.
- A small jaw and narrow roof of the mouth. This can cause teeth to become crowded, leading to tooth deformities, muscle spasms of the jaw, chewing difficulties, and breathing problems.
- Teeth with thin enamel and abnormal dentin (under the enamel). Despite this, cavities are less common in those with TS than in the general population.
- Gingivitis (inflammation of the gums), which is common in adults.
A pediatric dentist should be seen by age 2 and an orthodontist by age 7. Annual dental check-ups and teeth cleanings should be performed. A bone density study is also recommended before dental/orthodontic procedures.
Skin Problems
Individuals with TS develop little to no acne. However, they may develop different skin problems.
Benign (non-cancerous) moles, or nevi, develop in 70% of females with TS. They may increase in size and number throughout childhood.
Keloid and hypertrophic scarring are also commonly reported in Turner syndrome. However, they usually occur after surgery on areas prone to developing keloid scarring, such as the chest (after heart surgery) and back of the neck (after surgical correction of neck webbing).
Vitiligo (loss of skin pigmentation) and alopecia areata (hair loss) may be 3 times more common in TS than in the general population. Psoriasis (an autoimmune disorder that causes the overproduction of skin cells) may be twice as common in patients with Turner syndrome than in the general population, often developing at a very early age.
TS can also affect the fingers and toes. Swelling can increase the surface area of the fingers, leading to unusual fingerprint patterns (dermatoglyphics). 40% of individuals with TS have been found to have an increased number of larger finger ridges.
Hemangiomas (benign tumors made up of newly formed blood vessels) are more common in girls with TS than in other children. These may appear on the skin as birthmarks (port-wine stains or “strawberry” marks) or in internal organs, such as the intestines, where they may burst and cause bleeding.
The Lymphatic System
One of the jobs of the lymphatic system is to work with the cardiovascular system to maintain fluid levels in the body.
Lymphedema occurs when the lymphatic system is not able to handle the body’s fluid load. This condition is present in about 70% of individuals with Turner syndrome, with the hands and feet most commonly affected. It develops in TS because the lymphatic system never fully developed before birth.
Babies affected by TS may experience fetal edema (swelling while in utero). Some are born with swelling of the hands and feet that persists throughout their lifetime. Others may never experience any swelling. The occurrence of lymphedema varies.
Lymphedema in TS that is seen at birth usually resolves without treatment by age 2. However, it may occur or recur at any age. Because of this, girls and women with TS need to learn how to minimize lymphedema. This may involve using support stockings, elevation, massage, compression bandaging, and gentle exercise.
Cancer
Three large studies have reported that the risk of cancer in general is similar to or slightly higher in TS. However, for breast cancer specifically, the risk may be decreased. Some studies suggest a 30% decreased risk of breast cancer in women with TS.
Approximately 5–6% of individuals with Turner syndrome are 45X/46XY mosaic. This pattern increases their risk of developing gonadoblastoma, a benign tumor of the reproductive organs (gonads). Because these tumors become cancerous more than 60% of the time, preventative removal of the ovaries is recommended for these children.
TS may also cause an increased risk of:
- Childhood brain tumors and meningiomas (risk increased 4 to 6 fold).
- Bladder cancer.
- Skin cancer (risk of malignant melanoma may increase 2 to 3 fold).
These risks might relate to genetic and hormonal factors or the effects of hormonal treatments given to women with TS.
Treatments for Turner Syndrome
Treating Turner Syndrome in Children
The key aspects of managing TS in children are:
- Cardiovascular monitoring.
- Treatment of congenital heart disease.
- Growth hormone therapy starting as early as 12 to 24 months.
- Estrogen therapy for sexual development.
- Preservation of bone mineral density.
- Social, emotional, and academic support.
Growth Therapy
The goal of growth hormone treatment is to help those afflicted with TS to achieve average height as early in life as possible and experience puberty along with their peers. These therapies center around the use of human growth hormone (HGH).
HGH therapy effectively increases final adult height in girls with TS. The mean adult height in patients with TS is 4’8” (140 cm), but with growth hormone and estrogen therapy, the average height increases to 5’ (150 cm).
Growth hormone therapy is effective as early as 9 months of age. Your doctor will likely recommend starting growth hormone therapy as soon as growth failure begins.
Recent guidelines recommend starting GH treatment at 4–6 years of age if the child:
- Has evidence of growth failure.
- Is already short or has a strong likelihood of short stature (e.g., short parents and, therefore, short predicted adult height).
Your doctor may continue therapy until a girl has reached a satisfactory height or until she is unlikely to grow further (bone age ≥14 years and growth <2 cm/year). GH therapy should be directed by a pediatric endocrinologist who monitors growth at regular intervals.
Therapy for Puberty
Up to 30% of girls with TS have some spontaneous pubertal development. However, the majority (90%) will go on to experience premature ovarian failure. For many, a delay in puberty can play a large role in self-esteem, anxiety, and social isolation.
In the past, pubertal induction (the starting of puberty with medical treatments) was delayed until 15 years of age to maximize height potential. Today, however, age-appropriate pubertal induction is recommended to avoid the potential long-lasting psychosocial effects of delayed puberty.
More recent evidence suggests that when you start estrogen hormone therapy at age 12, you are more likely to experience puberty with your peers without compromising your adult height potential.
Transdermal 17-β estradiol (estrogen patch) is now the preferred estrogen treatment starting around age 11–12 years. Absorbing estrogen through the skin is more physiological than taking tablets. Hormone replacement is usually started at one-tenth to one-eighth of the adult dose and gradually increased over the course of two to four years.
Progesterone hormone treatment is then started once menses (menstruation) occurs or after about two years of estrogen therapy to minimize the risk of uterine cancer. Estrogen replacement is usually required until the time of menopause to maintain feminization and prevent osteoporosis.
Pubertal induction should be performed in consultation with an endocrinologist.
How Is TS Treated in Adults?
Adult women with TS require careful medical follow-up. Early medical intervention can substantially decrease your morbidity (disease burden) and mortality (risk of death) and improve your quality of life.
A multidisciplinary team should include specialists in endocrinology, cardiology, ear-nose-throat (ENT), infertility, gynecology, and psychology.
An adult woman with TS requires regular screening for:
- Osteoporosis
- Vitamin D levels
- Hypertension
- Diabetes
- Abnormal cholesterol
- Cardiovascular disease
- Aortic dilatation
- Thyroid and celiac disease
- Hearing loss
- Ongoing hormonal therapy
Fertility and Family-Planning Issues for Women With TS
Most women with TS experience infertility. Occasionally, however, a spontaneous pregnancy occurs.
Assisted reproductive technologies (donor eggs, in vitro fertilization) are usually required in order to conceive. Recent studies show that women with TS who undergo infertility treatments become pregnant as easily as women without TS. They can also carry their pregnancies to term without an increased miscarriage rate. This is encouraging.
That said, TS is associated with an increased risk of pregnancy complications due to:
- Small stature: small stature is often associated with a small pelvis, making vaginal delivery difficult. Cesarean section is more likely to occur. Stocky body shape also increases the risk of diabetes and hypertension-related diseases of pregnancy (preeclampsia).
- An increased risk for dilatation and dissection of the aorta during pregnancy.
Aortic dissection is a potentially serious pregnancy complication in women with TS. There is a high risk of death. Strict control of blood pressure and judicious cardiac monitoring is required for all pregnant patients with TS.
A multidisciplinary team of healthcare providers should monitor the pregnancy, including:
- High-risk obstetricians
- Cardiologists
- Reproductive endocrinologists
Before becoming pregnant, women with TS should undergo a complete medical evaluation. This includes testing for thyroid disease and diabetes, as well as a cardiac work-up. Women with certain heart conditions (bicuspid atrial valve, dilated aorta, or history of coarctation of the aorta) are advised against becoming pregnant or are recommended to consider the use of a gestational carrier.
Due to the increased risk of early menopause, women with TS who have functioning ovaries should not delay pregnancy. Consideration should be given to egg freezing.
The Bottom Line
Turner syndrome affects one out of every 2,500 live female births. It can affect multiple organs through all stages of life. Because of this, girls and women with TS require multidisciplinary care from a team of specialists.
There have recently been numerous important advances in the specialty fields concerning the care of girls and women with TS. As a result, the outlook for those diagnosed with TS has improved significantly over the past two decades. With the right medical and psychological care and the emotional support of friends and family, a girl with TS may look forward to a healthy, productive life.
Written by: Lisa Shephard, MD | Editor: Victoria Menard and Dayna Smith MD | Reviewed March 24, 2022 | Copyright myObMD. Media, LLC, 2022
References
- S. National Library of Medicine. (2020, September 8). Turner syndrome: MedlinePlus Genetics. MedlinePlus. Retrieved from: https://medlineplus.gov/genetics/condition/turner-syndrome/
- S. National Library of Medicine. (2021, November 16). Amniocentesis (amniotic fluid test): MedlinePlus medical test. MedlinePlus. Retrieved from: https://medlineplus.gov/lab-tests/amniocentesis-amniotic-fluid-test/
- Fergus, K. (2020, January 3). An Overview of Karyotyping: Karyotype’s Role in Diagnosis and Prenatal and Predictive Screening. Verywell Health. Retrieved from: https://www.verywellhealth.com/what-is-a-karyotype-1120441
- S. National Library of Medicine. (2021, November 16). Amniocentesis (amniotic fluid test): MedlinePlus medical test. MedlinePlus. Retrieved from: https://medlineplus.gov/lab-tests/amniocentesis-amniotic-fluid-test/
- S. National Library of Medicine. (n.d.). Chorionic villus sampling: MedlinePlus Medical Encyclopedia Image. MedlinePlus. Retrieved from: https://medlineplus.gov/ency/imagepages/9181.htm
- S. National Library of Medicine. (2022, January 27). Primary Ovarian Insufficiency. MedlinePlus. Retrieved from: https://medlineplus.gov/primaryovarianinsufficiency.html
- S. National Library of Medicine. (2021, July 7). Karyotype genetic test: MedlinePlus medical test. MedlinePlus. Retrieved from: https://medlineplus.gov/lab-tests/karyotype-genetic-test/
- Mayo Foundation for Medical Education and Research. (2021, September 10). In vitro fertilization (IVF). Mayo Clinic. Retrieved from: https://www.mayoclinic.org/tests-procedures/in-vitro-fertilization/about/pac-20384716
- American College of Cardiology. (2016). Congenital Heart Defects (CHD). CardioSmart. Retrieved from: https://www.cardiosmart.org/docs/default-source/assets/infographic/congenital-heart-defects.pdf?sfvrsn=cabc831b_2
- American Heart Association. (2021, January 22). Your Aorta: The Pulse of Life. Heart.org. Retrieved from: https://www.heart.org/en/health-topics/aortic-aneurysm/your-aorta-the-pulse-of-life
- Centers for Disease Control and Prevention. (2022, January 24). Congenital Heart Defects – Facts About Coarctation of the Aorta. Centers for Disease Control and Prevention. Retrieved from: https://www.cdc.gov/ncbddd/heartdefects/coarctationofaorta.html
- American Heart Association. (2020, May 8). Problem: Heart Valve Stenosis. Heart.org. Retrieved from: https://www.heart.org/en/health-topics/heart-valve-problems-and-disease/heart-valve-problems-and-causes/problem-heart-valve-stenosis
- S. National Library of Medicine. (2020, December 28). Pulmonary Hypertension. MedlinePlus. Retrieved from: https://medlineplus.gov/pulmonaryhypertension.html
- S. National Library of Medicine. (n.d.). Aortic Dissection: MedlinePlus Medical Encyclopedia. MedlinePlus. Retrieved from: https://medlineplus.gov/ency/article/000181.htm
- Traumatic Aortic Transection (Aortic Rupture). Cedars Sinai. (n.d.). Retrieved from: https://www.cedars-sinai.org/health-library/diseases-and-conditions/t/traumatic-aortic-transection-aortic-rupture.html
- Herndon, J. (2021, October 27). What Are the Causes and Symptoms of Preeclampsia? Retrieved from: https://www.healthline.com/health/preeclampsia
- S. National Library of Medicine. (n.d.). Developmental dysplasia of the hip: MedlinePlus Medical Encyclopedia. MedlinePlus. Retrieved from: https://medlineplus.gov/ency/article/000971.htm
- S. National Library of Medicine. (n.d.). Scoliosis: MedlinePlus Medical Encyclopedia. MedlinePlus. Retrieved from: https://medlineplus.gov/ency/article/001241.htm
- S. National Library of Medicine. (n.d.). Kyphosis: MedlinePlus Medical Encyclopedia. MedlinePlus. Retrieved from: https://medlineplus.gov/ency/imagepages/9499.htm
- S. National Library of Medicine. (n.d.). Lordosis: MedlinePlus Medical Encyclopedia. MedlinePlus. Retrieved from: https://medlineplus.gov/ency/imagepages/9583.htm
- S. National Library of Medicine. (n.d.). Osteoporosis: MedlinePlus Medical Encyclopedia. MedlinePlus. Retrieved from: https://medlineplus.gov/ency/article/000360.htm
- American College of Cardiology. (2016). Metabolic Syndrome. CardioSmart. Retrieved from: https://www.cardiosmart.org/docs/default-source/assets/infographic/metabolic-syndrome_final.pdf?sfvrsn=9154c920_7
- S. National Library of Medicine. (2020, August 18). Congenital anomalies of kidney and urinary tract: MedlinePlus Genetics. MedlinePlus. Retrieved from: https://medlineplus.gov/genetics/condition/congenital-anomalies-of-kidney-and-urinary-tract/
- Cristol, H. (2020, October 7). What Is Horseshoe Kidney? Grow by WebMD. Retrieved from: https://www.webmd.com/baby/horseshoe-kidney-renal-fusion
- Duplex Kidney. Cleveland Clinic. (2020, December 4). Retrieved from: https://my.clevelandclinic.org/health/diseases/16492-duplex-kidney
- Multicystic dysplastic kidney. Children’s Wisconsin. (n.d.). Retrieved from: https://childrenswi.org/medical-care/fetal-concerns-center/conditions/infant-complications/multicystic-dysplastic-kidney
- S. Department of Health and Human Services. (2019, September). Ectopic Kidney. National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved from: https://www.niddk.nih.gov/health-information/kidney-disease/children/ectopic-kidney
- S. National Library of Medicine. (n.d.). Vesicoureteral reflux: MedlinePlus Medical Encyclopedia Image. MedlinePlus. Retrieved from: https://medlineplus.gov/ency/imagepages/19502.htm
- S. National Library of Medicine. (2021, October 28). Autoimmune Diseases | Autoimmune Disease Symptoms. MedlinePlus. Retrieved from: https://medlineplus.gov/autoimmunediseases.html
- S. Department of Health and Human Services. (2021, June). Hashimoto’s Disease. National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved from: https://www.niddk.nih.gov/health-information/endocrine-diseases/hashimotos-disease
- S. National Library of Medicine. (2022, January 26). Hypothyroidism | Hashimoto’s Disease. MedlinePlus. Retrieved from: https://medlineplus.gov/hypothyroidism.html
- S. National Library of Medicine. (2020, August 18). Celiac Disease: MedlinePlus Genetics. MedlinePlus. Retrieved from: https://medlineplus.gov/genetics/condition/celiac-disease/
- Juvenile Rheumatoid Arthritis. Cedars-Sinai. (n.d.). Retrieved from: https://www.cedars-sinai.org/health-library/diseases-and-conditions/j/juvenile-rheumatoid-arthritis.html
- Rosario, J. F. del (Ed.). (2021, September). Inflammatory Bowel Disease (for teens). Nemours TeensHealth. Retrieved from: https://kidshealth.org/en/teens/ibd.html
- S. National Library of Medicine. (n.d.). Astigmatism: MedlinePlus Medical Encyclopedia. MedlinePlus. Retrieved from: https://medlineplus.gov/ency/article/001015.htm
- Boyd, K. (2021, November 24). What Is Adult Strabismus? American Academy of Ophthalmology. Retrieved from: https://www.aao.org/eye-health/diseases/what-is-strabismus
- S. Department of Health and Human Services. (2019, July 2). Amblyopia (Lazy Eye). National Eye Institute. Retrieved from: https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/amblyopia-lazy-eye
- S. National Library of Medicine. (n.d.). Eyelid drooping: MedlinePlus Medical Encyclopedia. MedlinePlus. Retrieved from: https://medlineplus.gov/ency/article/001018.htm
- Bourgeois, A. J. (Ed.). (2020, November). Your Child’s Vision (for Parents). Nemours KidsHealth. Retrieved from: https://kidshealth.org/en/parents/vision.html
- S. National Library of Medicine. (n.d.). Adult cataract: MedlinePlus Medical Encyclopedia. MedlinePlus. Retrieved from: https://medlineplus.gov/ency/article/001001.htm
- Parkes, W. J. (Ed.). (2017, April). Middle Ear Infections (Otitis Media) (for Parents). Nemours KidsHealth. Retrieved from: https://kidshealth.org/en/parents/otitis-media.html
- Acne and other follicular disorders. DermNet NZ. (1999). Retrieved from: https://dermnetnz.org/topics/acne-and-other-follicular-disorders/
- Melanoma. DermNet NZ. (2015, December). Retrieved from: https://dermnetnz.org/topics/melanoma/
- Oakley, A. (2015, August). Vitiligo. DermNet NZ. Retrieved from: https://dermnetnz.org/topics/vitiligo
- Oakley, A. (2015, December). Alopecia areata. DermNet NZ. Retrieved from: https://dermnetnz.org/topics/alopecia-areata/
- Oakley, A. (2020, December). Psoriasis. DermNet NZ. Retrieved from: https://dermnetnz.org/topics/psoriasis/
- Zheng, K. (2015, June). Fingerprints. DermNet NZ. Retrieved from: https://dermnetnz.org/topics/fingerprints
- Hirsch, L. (Ed.). (2021, February). The Lymphatic System (for Parents). Nemours KidsHealth. Retrieved from: https://kidshealth.org/en/parents/spleen-lymphatic.html
- Turner Syndrome Society of the United States. (n.d.). Turner Topic: A Patient Guide to Lymphedema and Turner Syndrome. Retrieved from: https://50edf458-92ec-48c8-96eb-0ee4183e817d.filesusr.com/ugd/8fb9de_e6fe3dcf4fe64653b3bde0ab4b33eb9c.pdf
- Bass, P. F. (Ed.). (n.d.). Germ Cell Tumors. Health Encyclopedia. Retrieved from: https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=90&contentid=p02725
- S. Department of Health and Human Services. (n.d.). Gonads. National Cancer Institute SEER Training Modules. Retrieved from: https://training.seer.cancer.gov/anatomy/endocrine/glands/gonads.html
- Mayo Foundation for Medical Education and Research. (2020, April 21). Meningioma. Mayo Clinic. Retrieved from: https://www.mayoclinic.org/diseases-conditions/meningioma/symptoms-causes/syc-20355643
- Melanoma Overview. The Skin Cancer Foundation. (2022, January). Retrieved from: https://www.skincancer.org/skin-cancer-information/melanoma/
- Mayo Foundation for Medical Education and Research. (2020, March 19). Preeclampsia. Mayo Clinic. Retrieved from: https://www.mayoclinic.org/diseases-conditions/preeclampsia/symptoms-causes/syc-20355745