The Pap Smear, Explained!
- What is a pap smear or pap test?
- What is HPV?
- When should I get my first pap test?
- How should I prepare for my pap test?
- How often should I get a pap test?
What is a Pap Smear or Pap Test?
Pap smears and pap tests are two names for the same procedure. The pap test is used to screen for cervical cancer. This means doctors use the test to check for cervical cancer in women with no symptoms. You may associate going to the gynecologist with getting a pap smear. While a pelvic exam is required for a pap test. Not all pelvic exams include a pap test.
Despite this being a common test, there is still a lot of surrounding confusion. How, when, and why is a pap smear performed are questions most women will have a difficult time answering. So, to demystify the pap smear, here is a summary of everything you need to know about this life saving, simple test called a pap.
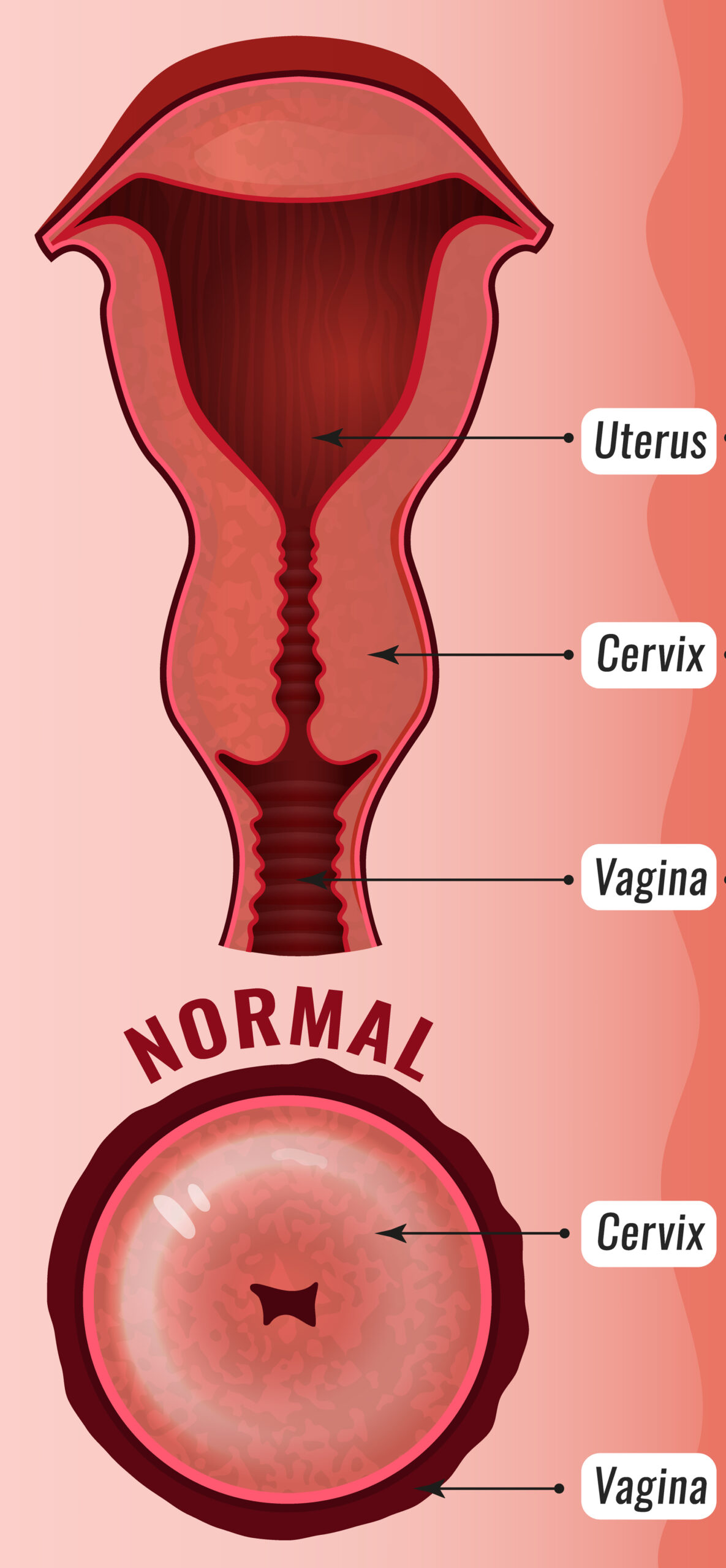
Named for the doctor who developed it, Dr. Georgios Papanikolaou, a “pap” smear is a small sample of the cells on the surface of the cervix. The cervix is the opening to the womb, or uterus. It is the portion that is the closest to the vagina. A pap smear test the cells within the cervix to determine if there are any cancer cells or cells which may go on to become cancer- precancer cells. When performing a pap smear, your doctor will gently place a device called a speculum in the vagina. The speculum opens and allows your doctor to see your cervix. You may feel some pressure or slight discomfort during this portion of the exam. The cells are collected with the use of a tiny brush or spatula and sent to the lab for analysis.
What is HPV?
Depending on your age, you may also have a human papillomavirus (HPV) test added to your pap smear. This is called co-testing. HPV is the virus that causes almost all cervical cancers. Also, HPV is the most common sexually transmitted disease, and most people are infected with HPV at some point in their lives. HPV infection has no symptoms, so you don’t know when you’ve been infected. The infection usually goes away without any treatment. In a few people, the infection can linger, causing the cells to become precancerous and sometimes even cancer. This is why getting a pap smear to detect these changes is so important. HPV testing occurs simultaneously with the pap smear and does not require any extra steps or additional time.
When Should I Get My First Pap Test?
In the US, pap smears begin at age 21. Earlier testing is not recommended as this leads to unnecessary procedures in young women. Plus, the risk of cervical cancer at that age is extremely low. The age at which you begin your pap testing has nothing to do with your sexual activity. Being sexually active before age 21 does not mean you should start testing early. Not being sexually active at age 21 does not mean you should delay getting a pap test. It is recommended that ALL women begin pap testing at age 21.
How Should I Prepare for My Pap Test?
To be sure your pap test results are accurate, it is best to optimize the timing of this test’s performance. In addition to avoiding testing while menstruating, there are other things you can do.
For two days before your pap test:
- Do not douche
- Avoid Intercourse
- Do not use vaginal medications
- Do not use vaginal hygiene products, such as tampons.
In general, do not place anything in the vagina for at least two days before your pap test. While it is best to schedule your pap in between your menstrual cycles, if you find yourself continually menstruating, you should have your pap rather than face a long delay.
How Often Should I Get a Pap Test?
The frequency of testing will vary according to your age and personal medical history. In general, the testing guideline recommends:
- Age 21, pap testing alone every three years.
- Age 30-65, pap and HPV co-testing every five years or a pap test alone every three years.
- Older than age 65, you may stop testing if you’ve never had an abnormal pap test, and your last three tests were normal.
There are exceptions to these guidelines. Your doctor may recommend a more aggressive testing regimen if you have any of the following conditions:
- HIV Positive
- Compromised Immune System
- History of Cervical cancer
- In utero exposure to diethylstilbestrol ( DES- a medicine prescribed to pregnant women 1940 through 1971).
If you have had a hysterectomy with removal of your cervix and no history or abnormal pap tests, you and your doctor will determine the best regimen for you. Your doctor may recommend a more relaxed screening regimen or even no screening. If you have received the HPV vaccine, you should still follow the screening guidelines. Thanks to pap testing, cervical cancer is an entirely preventable illness. You and your doctor will decide on the appropriate testing interval for you.
Copyright: myObMD Media, LLC | Written by Kerry E. Krauss, MD April 8, 2020 | Edited by Dayna Smith MD October 26, 2020
References
- Perkins, R et al. 2019 ASCCP Risk-Based Management Consensus Guidelines for Abnormal Cervical Cancer Screening Tests and Cancer Precursors. Journal of Lower Genital Tract Disease, April 2020, Volume 24. Issue 2 p. 102-131.
- Laprise JF, Chesson HW, Markowitz LE, Drolet M, Martin D, Bénard É, Brisson M. Effectiveness and Cost-Effectiveness of Human Papillomavirus Vaccination Through Age 45 Years in the United States. Ann Intern Med. 2019 Dec 10.
- American College of Obstetrics and Gynecolgy, Mutch, David, Why Annual Pap Smears are History but Routine Ob/Gyn visits are not. October, 2020
- American College of Obstetrics and Gynecology, Cervical Cancer Screening, Frequently Asked Questions, FAQ085, Published September, 2017; Last Reviewed April, 2018.
- Centers for Disease Control and Prevention. Cervical Cancer. What Should I Know About Screening? Page Last Reviewed August 7, 2019.