Endometriosis: Your Complete Guide: Endo Symptoms, Diagnosis, Treatment
- What is Endometriosis?
- Endometriosis Symptoms
- What Causes Endometriosis?
- How is Endometriosis Diagnosed?
- Treatment Options for Endometriosis
- Endometriosis Staging
- Treating Infertility Caused by Endometriosis
- What Can I Do To Treat Endometriosis On My Own?
- Is There a Risk of Developing Cancer with Endometriosis?
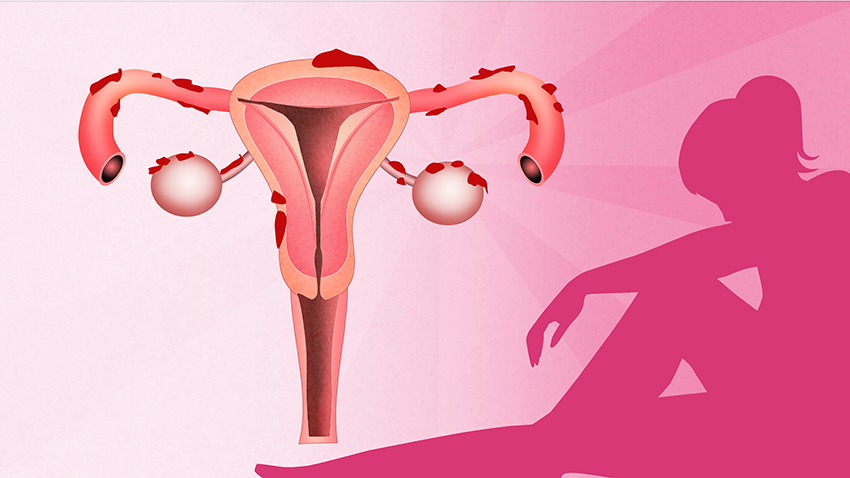
What is Endometriosis?

Endometriosis, or endo, is a medical condition where endometrial tissue is found outside of the uterus. To be clear, endometrial tissue normally lines the uterine wall. In most cases, misplaced endometrial tissue grow along the backside of the uterus, around the ovaries, and in other areas of the pelvis. In more rare cases, endometrial tissue may also grow in structures like the bowel (intestine), lungs, and abdominal wall. Further, areas of endometrial tissue growing outside the uterus are called endometrial implants.
Endometriosis Symptoms
In most cases, pain is the most common symptom of endometriosis. However, it usually varies in frequency and severity. Sometimes, women with endometriosis have no symptoms. But, many experience:
- Chronic pelvic pain, which gets worse over time.
- Painful periods (dysmenorrhea).
- Heavy menstrual periods.
- Intercourse that causes pain (dyspareunia).
- Bowel movements that cause pain.
- Difficulty getting pregnant (infertility).
What Causes Endometriosis?
It’s unclear what causes endometriosis. But, as it frequently runs in families, a genetic link is likely. Some experts believe that retrograde menstruation is the cause. Oftentimes, this occurs when menstrual fluid flows backward through the fallopian tubes and into the pelvic cavity. Usually, periods flow through the cervix and into the vagina. However, other theories suggest that cells from the uterus can travel to other parts of the body. And finally, a third theory is that cells in other parts of the body can turn into endometrial cells. Because most cases of endometriosis are found in the pelvis, the retrograde menstruation theory is the most commonly held theory.
- Hereditary – inherited at birth.
- Retrograde Menstruation – menstrual flow up and out of the fallopian tube instead of down into the vagina.
- Lymphatic or Hematogenous Transport – spread through the lymphatic or blood.
- Coelomic Metaplasia (pron. seal-oh-mic met-a-play-sha) – cells transform into endometrial cells.
How is Endometriosis Diagnosed?
Sometimes, endometriosis is hard to diagnose. Usually, a diagnosis depends on your reported symptoms, a pelvic exam, and an ultrasound. Then, the doctor provides a course of treatment. And, if that treatment works, it confirms the diagnosis of endometriosis.

Laparoscopic surgery
If you do not respond to the advised treatment, a confirmed diagnosis may require a surgical laparoscopy and biopsy. If found during a laparoscopy, the following may show signs of endometriosis:
- Endometriomas (“chocolate cysts”): Ovarian cysts filled with a fluid that looks similar to melted chocolate.
- Pelvic adhesions (scar tissue): Inflammatory bands that can cause organs and other tissues to stick together.
- Visible endometrial implants: Clumps of endometrial tissue in your pelvis seen by your doctor.
Treatment Options for Endometriosis
Treatment is specific to you and your symptoms.
Treating Pain and Heavy Periods Caused by Endometriosis
The following medications may be prescribed:
- NSAID (non-steroidal anti-inflammatory drug) pain relievers.
- Hormonal suppression therapy. Usually, this type of therapy helps to curb the growth of endometrial implants. And, it helps to prevent new ones from forming. This may include:
- Oral contraceptives (birth control pills).
- Progesterone or progestin. Sometimes, it comes as a pill or gel. Or, there are other forms of birth control method like an IUD (such as Mirena® or Skyla®), injection (Depo-Provera®), or implant (Nexplanon®).
- Androgen (Danazol).
- GnRH (gonadotropin-releasing hormone) agonist, like Lupron®.

If medication does not relieve pain, surgery may be the next step. Usually, women have different levels of relief following surgery. Unfortunately, few women feel total relief from pain. And, the effects of surgery may not last long. Additionally, some endometrial implants may be hard to find and remove. Finally, those that are removed may grow back in the future.
Surgical procedures performed for endometriosis may involve:
- Removing endometriomas (chocolate cysts).
- Dissecting or cutting away pelvic adhesions.
- Taking out the uterus (hysterectomy).
- Removing the uterus, and one or both ovaries (hysterectomy with oophorectomy).
Endometriosis Staging
Surgery serves to either diagnose or treat your endometriosis. In this case, your doctor describes what is called endometriosis staging. For one, endometriosis staging ranges from stage one, which is mild, through stage four (severe). In detail, it describes the visible extent of your endometriosis on your pelvic organs and bowels. On one hand, stage one endometriosis describes minimal endometriosis visible in your pelvis. On the other hand, stage four describes endometriosis that involves your pelvic organs and maybe your intestines. While stage four endometriosis usually links to severe symptoms and infertility, this is not always the case. For instance, you may have stage four endometriosis with mild or no symptoms. Or, you may have stage one endometriosis with severe symptoms. Overall, the purpose of endometriosis staging is for surgeons to describe their surgical findings. In short, endometriosis staging does not have to correlate with your symptoms.
Treating Infertility Caused by Endometriosis
Though infertility with endometriosis is common, it’s very treatable. Couples who have been unable to conceive after 12 months of regular unprotected sex (or after 6 months, if the woman is over age 35) should speak with their gynecologist. Sometimes, women with endometriosis who are having trouble conceiving may need one of the following:
- Surgery: For some patients, surgical removal of scar tissue, endometriomas (chocolate cysts), and/or endometrial implants are all that they need to conceive naturally. In most cases, patients that get pregnant after surgery have a mild case. Or, their endometriomas will most likely not come back. But, repeated surgeries as a way to help achieve pregnancy can cause more harm than good. Thus, doctors advise against it. In general, each time portions of the ovary are removed, your lifetime oocyte (or egg) production lowers. This is true for all patients, not just those with endometriosis.
- In-vitro fertilization (IVF): Usually, IVF is a last resort. Oftentimes, it is for patients whose surgery did not work. Or, it is for those with severe disease. Now, one of the biggest factors that impacts the success of IVF treatments is the age of the (female) patient. If this is an option that you want to try, you should act sooner rather than later. Because the sooner you start this process, the greater your chance of success. To explain, in the IVF procedure, fertilization occurs outside of the body. First, your doctor collects eggs and sperm from both parents. Then, your doctor fertilizes the eggs in the lab. Finally, the doctor implants the fertilized egg(s) into the mother’s uterus to grow.
What Can I Do To Treat Endometriosis On My Own?
There are very few daily habits that affect whether a woman will develop endometriosis, or how severe her symptoms will be. But, there is some evidence that these habits may affect endometriosis:
- Tobacco cessation: Quit smoking. In some cases, chewing tobacco/snuff may improve the symptoms of endometriosis.
- Breastfeeding: Sometimes, longer durations of breastfeeding decrease the risk of endometriosis.
- Regular exercise: Four or more hours per week may help ease symptoms.
Is There a Risk of Developing Cancer with Endometriosis?
There is concern that endometriomas on the ovaries carry a small risk of becoming cancerous. So, doctors recommend removing large, persistent, or growing endometriomas to limit the risk of cancer.
Written by: myObMD team |Editor: Dayna Smith MD |Reviewed: June 30, 2020
Copyright: myObMD, 2020
Endometriosis Glossary:
Chronic Pelvic Pain
Chronic pain is a term used to describe pain that is constant. It is there all the time. When this occurs in the pelvis, which is the area directly above your pubic bone, it is called chronic pelvic pain. Usually, the pain may wax and wane. At times mild, other times severe. But it is present most of the time.
Painful Periods (Dysmenorrhea; pron dis-men-oo-ree-ah)
While a painful period is more the norm than the exception with menses, the pain can range from mild to severe. For example, mild pain does not require any pain medicine or is easily relieved with pain medicine. Thus, it does not require medical intervention. For painful periods that impact with your quality of life, medical intervention may be needed. Interference with quality of life means the condition causes a disruption to your daily life activities. To explain, if your painful periods cause absence or issues with your work, school or relationships then medical intervention may be necessary.
Heavy Menstrual Periods
While the term “heavy” menstrual periods is subjective, there are some clear indicators of excessive bleeding with menses. For example, your period is heavy, and you should seek medical attention if you:
- Require two or more pads at a time, or a tampon and a pad at the same time.
- Need more than 2 pads in an hour.
- Use overnight pads; urinary incontinence pads; or towels, washcloths, etc. as sanitary napkins.
- You feel faint, dizzy, weak, cannot stand, or perform your normal daily functions.
Pain During Intercourse (Dyspareunia)
Painful intercourse encompasses many things. Sometimes pain may occur on the outer part of the vaginal area, known as the vulva. While other may have pain at the very tip of the vagina, or the vaginal opening. Or, there may only be pain with deep penetration at the very end of the vagina. Depending on where your pain is occurring, the evaluation and treatment may be different, as the causes are different. Still, pain during intercourse that occurs with endometriosis tends to be pain with deep penetration.
Infertility
Couples who have been unable to conceive after 12 months of regular unprotected intercourse (or after 6 months, if the patient is over age 35) suffer from infertility. Causes range from female factors, male factors or unknown.
Laparoscopy (pron. lap-oh-ras-copy)
Laparoscopy is a surgical procedure that involves a small (usually 10-12mm) incision right above or below the navel. However, there may be additional small incisions as needed. A camera and tools are placed through the incision(s) that allow the surgeon to operate. As a result, laparoscopic surgeries are minimally invasive. So, you recover faster and have less pain than with traditional surgeries. In most cases, patients can go back to work or school after 1-2 weeks.
Biopsy (pron. bye-op-see)
A biopsy is a procedure where a small sample of tissue is cut. Then, a pathologist reviews it after its delivery. To be clear, a pathologist is a physician that looks at the tissue under the microscope. Then, they determine what, if any, disease process there may be at a microscopic level.
Ovarian Cyst
The ovary is the small, pearl colored organ that hangs between the uterus and fallopian tubes. While you only need one to function, most folks have two, one on each side. Each month the ovaries release eggs that swim about looking for sperm to be fertilized (pregnant). When we do not get pregnant, the ovaries dissolve. And, we get a period. Then, the eggs are housed in these fluid filled cavities called cysts. Usually, these cysts are no bigger than a small grape (3-4cm in diameter). However, in some cases, the cysts grow large and are painful. Also, larger cysts can pop. And, this can again be painful. But, you most likely have no symptoms from a small cyst. Oftentimes, they go undetected. Yet, larger cysts usually cause you to seek medical attention. In most cases, extreme pain or your tummy growing are key signs of an ovarian cyst.
NSAID (pron. en-said)
NSAIDS, or non-steroidal anti-inflammatory drugs, are a group of drugs that are very commonly used in gynecology. For example, common over the counter NSAIDs are ibuprofen, naprosyn and aspirin. They work great because they help to relax the uterus. Thus, related pain lessens. But, using too much can cause damage to the lining of the stomach (stomach or gastric ulcers) and the kidneys. And, people who are pregnant or taking blood thinners should not use them. Additionally, patients with hypertension should use them with caution.
Oral Contraceptive Pills (OCP)
The original goal of OCP, or birth control pills, was to prevent pregnancy. However, their use involves way more than just keeping you from getting pregnant. Now, patients use them to treat acne, painful periods, heavy periods, and ovarian cysts. In most cases, OCP consist of two hormones: estrogen and progesterone. In general, OCP is safe for most women.
Progesterone (pron. pro-jes-tay-rhone)
Progesterone is one of the hormones used in OCP. This treatment is an option if you:
- Cannot or do not want to take the estrogen found in OCP.
- Do not want to take a pill.
There are many forms of progesterone. For example, there is a pill, an injection, an IUD, or a rod placed in your arm (Nexplanon®).
Androgen (Danazol®/Gestrinone®)
Androgens are steroidal hormones that are very effective. But, they are very rarely used in gynecology. Because of their risks of serious side effects, most doctors opt for safer treatment methods.
GnRH (pron. gee-en-r-h) Agonists
GnRH stands for gonadal releasing hormone. The more commonly used GnRH agonist is a drug called Lupron®. Further, GnRH is an injection. Either the injection is a large dose at one time. Or, it is a smaller doses over a three month period. Either way, this drug greatly lessens the amount of estrogen in your body. Thus, it creates what some refer to as a “medical menopause.” However, the drug can have side effects of hot flashes. And, there is a chance of your bones weakening. Usually, the drug is for short-term use. Depending on your length of treatment or severity of symptoms, your doctor may add another hormone to “add-back” the hormone depletion caused by the drug.
References
- American College of Obstetrics and Gynecology Practice Bulletin Number 114, July 2010 Management of Endometriosis
- Zondervan, Krina D Phil, Becker, Christian MD, Missmer, Stacey Sc.D Endometriosis, Review Article, N Engl J Med 2020; 1244-1256