Heavy, Prolonged Periods (Menorrhagia) Symptoms, Treatments, and More
- Key Takeaways
- What Is Menorrhagia (Heavy Periods)?
- How Do I Know if I Have Menorrhagia?
- Why Am I Having Heavy Periods?
- How Is Menorrhagia Diagnosed?
- Treatments for Abnormally Heavy Periods
- How Do I Decide Which Treatment Is Best for Me?
Key Takeaways
- Menorrhagia refers to heavy or prolonged menstruation that interferes with your life.
- There are many different causes of menorrhagia, including conditions that affect the uterus, hormone imbalances, and other medical problems.
- Heavy and prolonged menses can be treated with hormonal or non-hormonal medications, or surgery.
What Is Menorrhagia (Heavy Periods)?
Menorrhagia is the medical term for heavy and/or prolonged menstrual periods. The Centers for Disease Control and Prevention (CDC) estimates that 1 in every 5 women, or over 10 million women in the US, suffer from abnormally heavy periods.
Heavy menses can impact your emotional, social, and physical quality of life. Heavy menstrual bleeding can cause absences from school or work, an increased financial burden (due to the need to purchase more sanitary products), and interfere with your ability to perform or enjoy normal day-to-day activities. In prolonged and severe cases, menorrhagia may even lead to blood loss that is significant enough to require a blood transfusion.
How Do I Know if I Have Menorrhagia?
Most women have a menstrual period every 24 to 38 days. It should last between 2 and 7 days, and the typical daily blood loss is 2 to 3 tablespoons of menstrual blood.
Signs That Your Periods are Abnormally Heavy:
- Bleeding that lasts more than 7–8 days.
- Bleeding that soaks through one or more tampons or pads every hour for several hours in a row and happens every time you get your period.
- Needing to wear more than one pad at a time, or a pad and tampon at the same time.
- Needing to change pads or tampons during the night.
- Menstrual flow with blood clots that are as big as a quarter or larger.
- Heavy menstrual flow that prevents you from doing the things you would normally do.
- Constant pain in the lower part of the stomach during your periods.
- Lack of energy, extreme tiredness, or shortness of breath.
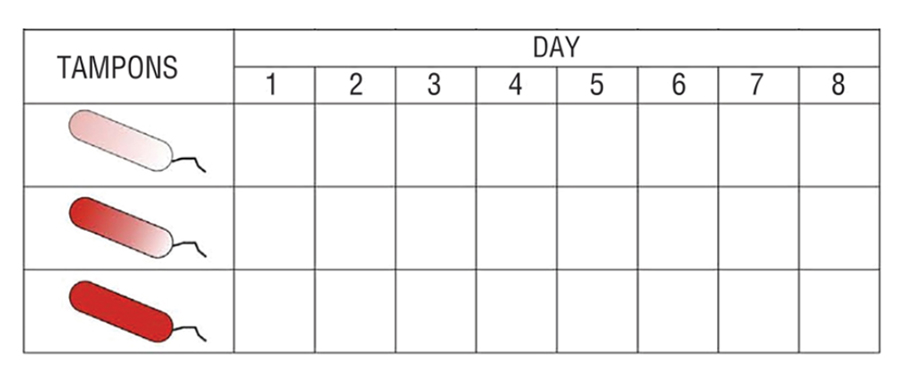
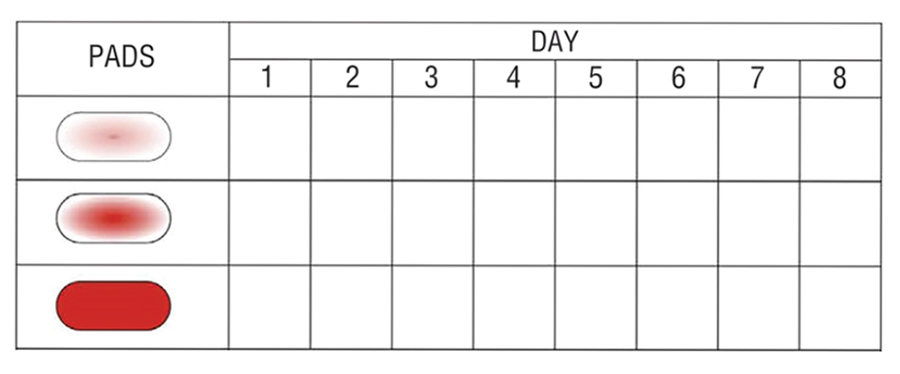
The following charts can help keep track of how much you bleed during your period. The numbers 1 to 8 represent the days of your menstrual period. For each day, record the number of pads you used that match each picture. If you’re concerned about the amount or duration of your period, you can bring these charts to your next appointment and show them to your provider.
How Do I Know if I Need to Go to the Emergency Room?
You should see your doctor or go to the emergency room right away if you soak through 4 or more pads or tampons in 2 hours. Additionally, you should seek emergency medical care if you are bleeding and are pregnant or think that you may be pregnant. Heavy bleeding during pregnancy may be a sign of a serious medical concern.
Go to the emergency room for vaginal bleeding that causes you to soak through four or more pads or tampons in two hours.
Why Am I Having Heavy Periods?
There are several reasons for having heavy menstrual cycles. We can group them into three main categories:
- Problems with the uterus
- Hormonal problems
- Medical problems
What Uterine Problems Cause Heavy Periods?
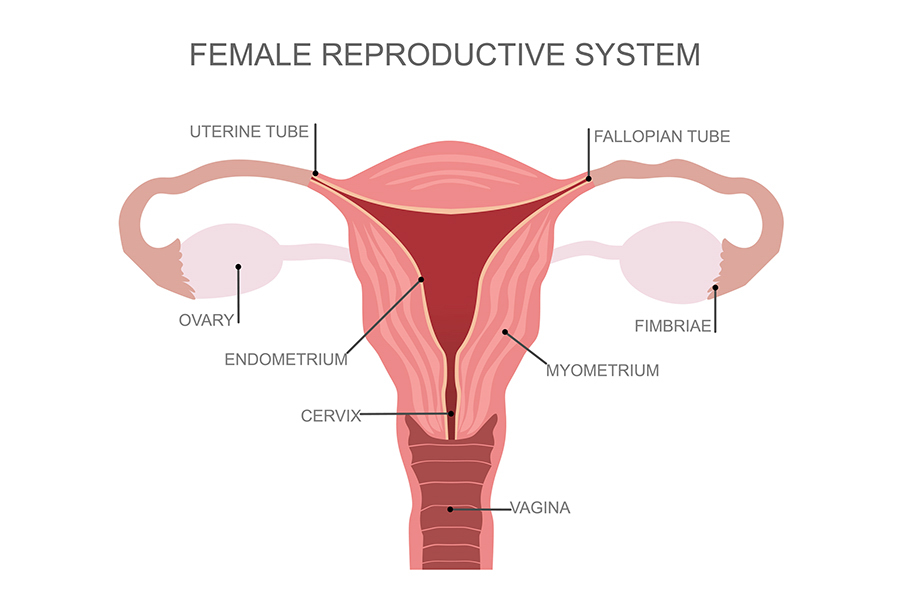
The uterus, or womb, is the hollow reproductive organ that houses and nourishes a baby during its development. Several problems with the uterus can lead to heavy periods, including:
-
- Growths and muscle cell tumors that are not cancerous. These are called polyps and fibroids.
- An intrauterine device (IUD).
- A problem pregnancy, such as an ectopic pregnancy or a miscarriage.
- Cancer of the uterus (endometrial cancer) or cervix (cervical cancer).
- An infection of the cervix or uterus, such as pelvic inflammatory disease (PID).
- Adenomyosis– boggy enlarged uterus.
- Endometriosis– cells that normally line the uterus are located outside the uterus.
Menstrual irregularities may be caused by problems with your uterus, hormones or medical issues.
What Hormonal Problems Cause Abnormally Heavy Menses?
In some cases, imbalances of certain hormones can cause heavy or prolonged menstrual bleeding. Some hormonal conditions that can cause menorrhagia include:
- An underactive thyroid gland (hypothyroidism).
- Ovulatory dysfunction– abnormal bleeding that occurs because you aren’t ovulating regularly. It is very common in adolescents who are just starting to get periods and in older women who are nearing menopause.
What Other Medical Problems Can Cause Heavy Menstrual Bleeding?
One common cause of menorrhagia are bleeding disorders that prevent the blood from clotting (sticking together) normally. Von Willebrand disease is one example. Up to 20% of women with menorrhagia are found to have a bleeding disorder.
Certain medications, such as blood thinners or hormonal birth control, can cause a person to experience heavier or longer menstrual bleeding than normal. Research has also shown a connection between obesity and heavy periods.
How Is Menorrhagia Diagnosed?
If you experience heavy or longer-than-usual menstrual bleeding, talk to a healthcare provider like your OB/GYN. They can determine the cause of heavy bleeding and work with you to find the best way of treating or managing it.
The first thing your provider will want to do is to take a thorough health history, which includes asking you about:
- Your menstrual history.
- At what age did your periods begin?
- How far apart are your periods?
- How long do your periods last?
- How heavy are your periods?
- A bleeding history.
- Do you bruise easily?
- Do you get frequent nosebleeds?
- Do your gums bleed easily?
- Does anyone in the family have bleeding problems?
- If you’ve had a baby, undergone surgery, or had dental work, did you bleed a lot afterward?
This can help your provider rule out certain potential causes of menorrhagia.
Recurrent heavy periods can cause severe anemia requiring blood transfusion.
Tests for Menorrhagia
After taking your health history, your provider will perform a pelvic exam. This involves:
- Taking a pap smear to check for abnormal/cancerous cells from the cervix.
- Performing a test for sexually transmitted infections (STIs) like gonorrhea and chlamydia.
Your provider may also want to take tissue samples from the inside lining of your uterus (called the endometrium). This is called an endometrial biopsy, and it checks for abnormal or cancerous cells inside the uterus.
Your doctor will also want to order blood work, including:
- A pregnancy test.
- A blood count to check for anemia.
- Thyroid tests.
- Bleeding studies, depending on your history.
- Labs to check for polycystic ovary syndrome (PCOS), depending on your history and examination.
Finally, a sonogram will be ordered. Sonograms, also called ultrasounds, use sound waves to create a picture of the uterus and ovaries. An ultrasound can detect ovarian cysts, endometrial polyps, and fibroids.
Treatments for Abnormally Heavy Periods
Depending on the results of your tests, your provider will discuss the next steps that should be taken. It is not uncommon for all of the diagnostic tests to come back normal. If no cause of your heavy menstrual bleeding is found, treatment would start with medications.
Hormonal Treatments
Hormonal medications include the birth control pill, patch, vaginal ring, shot (injection in your muscle), and certain IUDs. These treatments reduce bleeding during your menstrual period and can also help reduce cramps and pain during menstruation. It can take up to 3 months for bleeding to improve after you start taking hormonal birth control.
Progestin Pills
Aygestin and Provera are the two most common progestin pills that may be prescribed. They are usually given for 5 to 14 days each month or continuously (every day). This treatment helps keep the lining of the uterus thinner, reducing (or even eliminating) menstrual bleeding.
Progestin Injections and Progestin Implants
There are several other different options for progestin treatments. Depo-Provera is a long-acting form of progestin. It is given as a shot (injection in your muschle) once every 3 months. Nexplanon is a progestin implant that is inserted under the skin of the upper arm. This treatment prevents pregnancy and can reduce heavy menstrual bleeding. It is best for women who do not want to become pregnant in the next year or more. The most common side effect is bleeding and spotting, especially in the first few months. Many women completely stop having menstrual periods after using nexplanon for one year.
Hormonal IUD
Intrauterine devices, or IUDs, work by slowly releasing progestin into the uterus. Two such devices are called Mirena and Liletta. This type of IUD prevents pregnancy and reduces menstrual bleeding for five or more years.
A healthcare provider places the IUD inside of your uterus. The procedure is performed in-office. The most common side effect is light bleeding or spotting, especially in the first few months.
Non-Hormonal Treatments
Antifibrinolytic Medication
Antifibrinolytic medications can slow menstrual bleeding quickly. These medicines work by helping the blood clotting system. Lysteeda (tranexamic acid) is an anti-fibrinolytic.
The advantages of antifibrinolytic medications are:
- They slow bleeding within 2–3 hours.
- You only need to take them for a few days each month.
- They do not interfere with getting pregnant.
- You can use them with nonsteroidal anti-inflammatory drugs (NSAIDs).
Side effects of antifibrinolytics can include headache, muscle cramps, or pain. You should not take antifibrinolytic medicines with hormonal birth control unless you first discuss it with your healthcare provider. This is because some research suggests a possible increased risk of blood clots, stroke, and heart attack when taken together.
Taken together, antifibrinolytics and hormonal birth control can cause an increased risk of blood clots, stroke and heart attack. Speak with your doctor about your treatment regimen.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
Nonsteroidal anti-inflammatory drugs, such as ibuprofen (Motrin or Advil) and mefenamic acid (Ponstel), can help reduce menstrual bleeding and menstrual cramps. You can buy NSAIDs (including ibuprofen) without a prescription.
Some of the advantages of NSAIDs are:
- They are not expensive.
- They have few side effects.
- They reduce pain and bleeding.
- You need to take them only during your menstrual period.
However, NSAIDs do not work as well as other medical treatments in reducing bleeding. In addition, prolonged use of NSAID can cause damage to your stomach and kidneys.
Gonadotropin-releasing Hormone (GnRH) Agonists
GnRH agonists are a type of medicine that can be used to temporarily reduce menstrual bleeding. This treatment might be recommended for women who are waiting to have a surgical treatment.
These medicines work by “turning off” the ovaries, causing temporary menopause. The medicines can be taken for up to 6 months. Side effects may include hot flashes and vaginal dryness, just as you would expect if you were in menopause. It is not recommended to take GnRH agonists for longer than six months due to the risk of weakening your bones when used for long periods of time.
Surgical Treatments
For women who have growths in the uterus, such as polyps or fibroids, removing the growth can reduce or stop heavy menstrual bleeding.
Polypectomy
Polypectomy is the name of the procedure to remove polyps inside the uterus. Studies have shown that when polyps are the cause of menorrhagia, 75–100% of women who have a polypectomy have lighter menstrual periods.
Fibroid Removal
Removal of fibroids can be performed in several ways.
- Myomectomy is the name of the surgical procedure to remove fibroids from the uterus. Note that in 10–25% of cases, fibroids will return after a myomectomy and another procedure will be required.
- Uterine artery embolization (UAE) cuts off the blood supply to the fibroids. UAE causes fibroids to shrink in size and become less active.
- Hysterectomy is the name of the surgical procedure to remove the uterus (not the ovaries). For women who don’t want future pregnancies, hysterectomy is the preferred method to stop menorrhagia and ensure that fibroids do not come back.However, hysterectomy is a major surgery. Though it cures heavy menstrual bleeding, It is a permanent, more invasive treatment and has a greater risk of complications. You may need up to 6 weeks for a full recovery. Note that pregnancy is not possible after a hysterectomy.
- Endometrial ablation is a minimally invasive treatment that removes/destroys most of the lining of the uterus. It can be performed in the office or as an outpatient surgery. After an endometrial ablation, you may have some cramping and 2 to 10 days of vaginal discharge. You should be able to go back to work or school the following day.There are a few important things to note about endometrial ablation:
- It can either reduce or completely stop menstrual bleeding.
- It is not an option for women who intend to become pregnant in the future. Birth control must always be used after having an endometrial ablation.
- It is not a good option for you if your heavy bleeding is caused by ovulatory problems or adenomyosis.
- It is important for your doctor to identify the cause of your heavy bleeding before performing an endometrial ablation.
- Endometrial ablation should not be performed if there is any question of precancerous or cancer cells in the uterus.
Treatment for heavy menstrual bleeding can include hormones, non hormones or surgery.
How Do I Decide Which Treatment Is Best for Me?
There are many treatments for heavy menstrual bleeding, and it can be hard to decide which one is right for you. You and your doctor should have a thorough discussion regarding all of your options, their risks, and their success rates.
In most cases, your doctor will recommend starting with medical treatment (medications). In general, a trial of medication for 3 to 6 months will allow you to decide if it will control your menorrhagia.
If you continue to have heavy menstrual bleeding, it is essential to follow up with your gynecologist so that you can discuss additional testing and other treatment options.
Written by: Lisa Shephard, MD | Editor: Victoria Menard and Dayna Smith MD | Reviewed November 18, 2022 | Copyright myObMD. Media, LLC, 2022.
References
- Higham JM, O’Brien PM, Shaw RW. Assessment of menstrual blood loss using a pictorial chart. British Journal of Obstetrics and Gynaecology. 1990;97:734–739. https://doi.org/10.1111/j.1471-0528.1990.tb16249.x
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 651: Menstruation in girls and adolescents: Using the menstrual cycle as a vital sign. Obstet Gynecol. 2015;126(6):e143-e146. doi:10.1097/AOG.0000000000001215
- American College of Obstetricians and Gynecologists. ACOG Committee on Practice Bulletins—Gynecology. No.128: Diagnosis of abnormal uterine bleeding in reproductive-aged women. Obstet Gynecol. 2012;120(1):197-206. doi:10.1097/AOG.0b013e318262e320
- American College of Obstetricians and Gynecologists. ACOG committee opinion no. 557: Management of acute abnormal uterine bleeding in nonpregnant reproductive-aged women. Obstet Gynecol. 2013;121(4):891-896. doi:10.1097/01.AOG.0000428646.67925.9a
- American College of Obstetricians and Gynecologists. ACOG committee opinion no. 785: Screening and management of bleeding disorders in adolescents with heavy menstrual bleeding. Obstet Gynecol. 2019;134(3):e71-e83. doi:10.1097/AOG.0000000000003411
- Berntorp E, Follrud C, Lethagen S. No increased risk of venous thrombosis in women taking tranexamic acid.Thromb Haemost. 2001;86(2):714.
- Darney P, Patel A, Rosen K, et al. Safety and efficacy of a single-rod etonogestrel implant (Implanon): Results from 11 international clinical trials. Fertil Steril. 2009;91(5):1646. Epub 2008 Apr 18.
- El-Nashar SA, Hopkins MR, Creedon DJ, et al. Prediction of treatment outcomes after global endometrial ablation. Obstet Gynecol. 2009;113(1):97.
- Jensen JT, Parke S, Mellinger U, et al. Effective treatment of heavy menstrual bleeding with estradiol valerate and dienogest: a randomized controlled trial. Obstet Gynecol. 2011;117(4):777.
- Munro MG, Critchley HO, Broder MS, et al. FIGO working group on menstrual disorders FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int J Gynaecol Obstet. 2011;113(1):3. Epub 2011 Feb 22.
- Nathani F, Clark TJ. Uterine polypectomy in the management of abnormal uterine bleeding: A systematic review. J Minim Invasive Gynecol. 2006;13(4):260.
- Preutthipan S, Herabutya Y. Hysteroscopic polypectomy in 240 premenopausal and postmenopausal women. Fertil Steril. 2005;83(3):705.
- Rees MC, DiMarzo V, Tippins JR, et al. Leukotriene release by endometrium and myometrium throughout the menstrual cycle in dysmenorrhoea and menorrhagia. J Endocrinol. 1987;113(2):291.
- Salim S, Won H, Nesbitt-Hawes E, Campbell N, et al.Diagnosis and management of endometrial polyps: a critical review of the literature. J Minim Invasive Gynecol. 2011 Sep;18(5):569-81. Epub 2011 Jul 23.
- Sharp HT. Assessment of new technology in the treatment of idiopathic menorrhagia and uterine leiomyomata. Obstet Gynecol. 2006;108(4):990.
- Sundström A, Seaman H, Kieler H, et al. The risk of venous thromboembolism associated with the use of tranexamic acid and other drugs used to treat menorrhagia: a case-control study using the General Practice Research Database. BJOG. 2009;116(1):91. Epub 2008 Nov 11.
- Thorne JG, James PD, Reid RL. Heavy menstrual bleeding: is tranexamic acid a safe adjunct to combined hormonal contraception [commentary]? Contraception. 2018;98:1–3.